Ear
 This is one of the most common questions heard by hearing healthcare specialists. The purpose of cerumen, or earwax, is to lubricate, clean, and protect the ear canal from bacteria, insects, and other foreign objects. For the most part, ears clean themselves. Cerumen typically works its way out of the ear canal naturally like a “conveyor belt” with assistance from jaw movement such as talking and chewing.
This is one of the most common questions heard by hearing healthcare specialists. The purpose of cerumen, or earwax, is to lubricate, clean, and protect the ear canal from bacteria, insects, and other foreign objects. For the most part, ears clean themselves. Cerumen typically works its way out of the ear canal naturally like a “conveyor belt” with assistance from jaw movement such as talking and chewing.
People who wear hearing aids are sometimes more susceptible to earwax buildup. Having a hearing aid in the ear all day, every day, can prevent the earwax from working its way out on its own. When earwax accumulates and blocks the ear canal, it can cause problems such as pain, itching, fullness, odor, drainage, and additional hearing loss.
If you do have excessive earwax DO NOT clean your ears with cotton swabs. Cotton swabs often push the earwax deeper into the canal which can be dangerous. The best way to treat excessive cerumen is to place a few drops of mineral oil into the ear for 1-2 minutes to help soften the earwax. Then, with your head tilted to the side, use an eyedropper to fill the ear with 3% hydrogen peroxide and let it sit for about one minute. This will “bubble” out the earwax that is present. For stubborn cerumen impactions, it may be necessary to see a professional to have it removed. Your professional can then determine the best course for long-term management.
Otosclerosis is a disorder of bone metabolism that affects only the ear.
The bone where the inner ear and the third hearing bone (stapes) meet is called the oval window. This is where otosclerosis affects the ear. Bone is constantly being broken down and rebuilt by our body. In otosclerosis, the rate of rebuilding is increased resulting in the formation of new bone at the oval window.
Hearing loss is the main symptom.
Unlike many problems with the ear that can cause hearing loss, ear drainage, infections, or dizziness, otosclerosis mainly causes hearing loss. Sometimes the hearing loss is accompanied by tinnitus (ringing in the ear or head noise). The hearing loss is usually conductive, meaning sound is blocked from reaching the inner ear. The inner ear, hearing nerve, and brain often process the limited sound that reaches them completely normally.
People affected by otosclerosis are usually born with normal hearing. They may develop hearing loss in their 20s but this can occur from teens to midlife. Women are more commonly affected than men.
Otosclerosis is inherited from your parents.
The pattern of inheritance is autosomal dominance. This means that if one parent has it, the children have a 50% chance of getting it. However, there is variable penetrance. This means that if you get the gene, you are only at risk for otosclerosis. There is no guarantee of hearing loss. The trigger may be a viral infection, such as measles. Although measles vaccine protects against contracting measles symptoms, it does not protect against triggering otosclerosis.
Deafness from otosclerosis is unlikely.
Because it typically only blocks the conduction of sound, there is a limit to the hearing loss that it can cause. It will progress until the hearing bones are completely stuck. At this point hearing loss is around 50%. It commonly does affect both ears in two out of three cases. Rarely, it progresses from the oval window into the inner ear. This is called cochlear otosclerosis. In these cases, it decreases processing of sound in the inner ear as well. In these instances, hearing loss is more severe.
If you have hearing loss, you need to first have a hearing test to find the cause.
A otolaryngologist (ear, nose, and throat specialist) will provide a hearing test and evaluation. They will examine your ear to check for other causes of hearing loss and evaluate your ability to hear a tuning fork to further differentiate your hearing loss.
The three options to treat otosclerosis are medical therapy, hearing aids, and stapes surgery.
The goal of medical therapy is to prevent the disease from advancing. Fluoride is one option. It prevents the buildup of new bone at the oval window. Bisphosphonates are a class of medications commonly used in osteoporosis. They decrease bone destruction. Since otosclerosis is a problem of bone breakdown and repair, they may help slow progression. Neither of these reverse the hearing loss that has already occurred.
Hearing aids are an option to treat many forms of hearing loss, including hearing loss caused by otosclerosis. They are a great option for patients who would like to hear better and prefer to avoid surgery or are not surgical candidates.
The goal of surgical therapy is to correct the conductive hearing loss associated with otosclerosis. During surgery, an incision is made in the ear canal allowing the surgeon to elevate the ear drum and look behind it. The stapes (third hearing bone) is removed and a prosthesis is placed to connect the incus (second hearing bone) and the inner ear. The ear drum is then returned to its normal position. The procedure is called a stapedotomy.
There are minor risks associated with any form of treatment.
Medications such as fluoride and bisphosphonates may cause stomach upset, allergic reaction, or joint pain. Rarely break down of the ear canal bone or jaw bone is a side effect.
Hearing aids are generally well tolerated. Occasional discomfort associated with poor fitting molds or ear wax buildup may be experienced.
General risks of surgery apply to stapedotomy surgery. Specific to the procedure, there is a 1% chance of hearing loss. After surgery, there may be a metallic taste in the mouth temporarily. Very rarely, injury to the facial nerve may occur.
Stapedotomy is preferred under normal circumstances.
Successful stapedotomy prevents further conductive hearing loss. It also allows the patient to have restored hearing without the use of a hearing aid. The risks are minimal. It is the usual option for patients who are candidates for surgery. For nonsurgical candidates, a hearing aid avoids all the risks of surgery and works very well to amplify the hearing loss at specific frequencies needed. Medical therapy is usually not the standard treatment as it only halts progression at best and does nothing to restore hearing loss caused by otosclerosis.
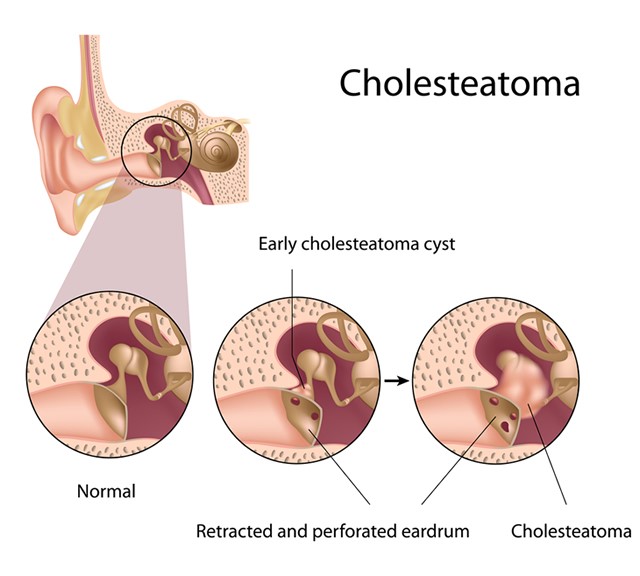 A cholesteatoma is a skin cyst that occurs in the middle ear.
A cholesteatoma is a skin cyst that occurs in the middle ear.When certain risk factors are present, the ear drum becomes floppy and retracted. This creates a pocket in the middle ear that collects skin cells and skin debris.
Certain risk factors create a favorable situation for cholesteatoma in your ear.
These include recurrent ear infections, chronic allergies, cigarette smoke, Eustachian tube dysfunction, and congenital abnormalities.
Symptoms that may indicate a cholesteatoma include hearing loss, recurring ear infections, and discharge from the ear canal.
The discharge may have a bad smell. It may also be discolored. Rarely, some cholesteatomas do not have symptoms and are noted on routine ear examination.
Visit your ENT doctor.
These symptoms do not necessarily indicate a cholesteatoma, but your doctor can examine your ear. In addition, they may recommend medical treatment, a hearing test.
You should see someone trained in ear surgery.
Although symptoms of cholesteatoma will respond to medical treatments such as antibiotics given by mouth or by ear drop, after treatment is completed symptoms will return. No medical treatment is available to reverse the changes seen in ears with cholesteatoma, and they usually need to be removed.
If left untreated, cholesteatomas will continue to grow.
As they enlarge, they damage the hearing bones resulting in worsening hearing loss. Further growth may damage the inner ear or balance system causing deafness or vertigo. Cholesteatomas that are allowed to grow many years can even destroy bone between the ear and brain leading to spinal fluid leak, herniated brain tissue, or meningitis.
An ear specialist who has surgical training in the delicate structures of the ear removes it during day surgery.
In a procedure known as tympanoplasty with mastoidectomy, the surgeon will remove the cholesteatoma. They will also repair the damage to the ear drum and hearing bones done by the cholesteatoma. This takes around 2 hours to complete.
Tympanoplasty with mastoidectomy is common.
It is usually performed in the outpatient setting, so you can go home the next day. The main risk of surgery is recurrence of cholesteatoma, so your surgeon must be very thorough. Even when cholesteatomas are completely removed, a new cholesteatoma can form if risk factors are not changed. In cases of extensive cholesteatoma, a second operation may be needed to ensure no residual cholesteatoma was left behind. Hearing loss, dizziness, and injury to structures surrounding the ear are rare risks to surgery as well.
CT scanning and facial nerve monitoring can make it safer.
In complex cases, CT scan is ordered before surgery to help predict variations in the surrounding structures and avoid injury. Also, facial nerve monitoring is used to enhance the safety of working around the facial nerve.
Generally, one to two days off work are needed to feel normal.
After that, you will typically have a postoperative appointment within 2 weeks of the operation. You avoid getting the ear wet until cleared by your surgeon. This usually takes about 6 weeks. You should not fly during this time. Hearing improves slowly over the 2 months following surgery.
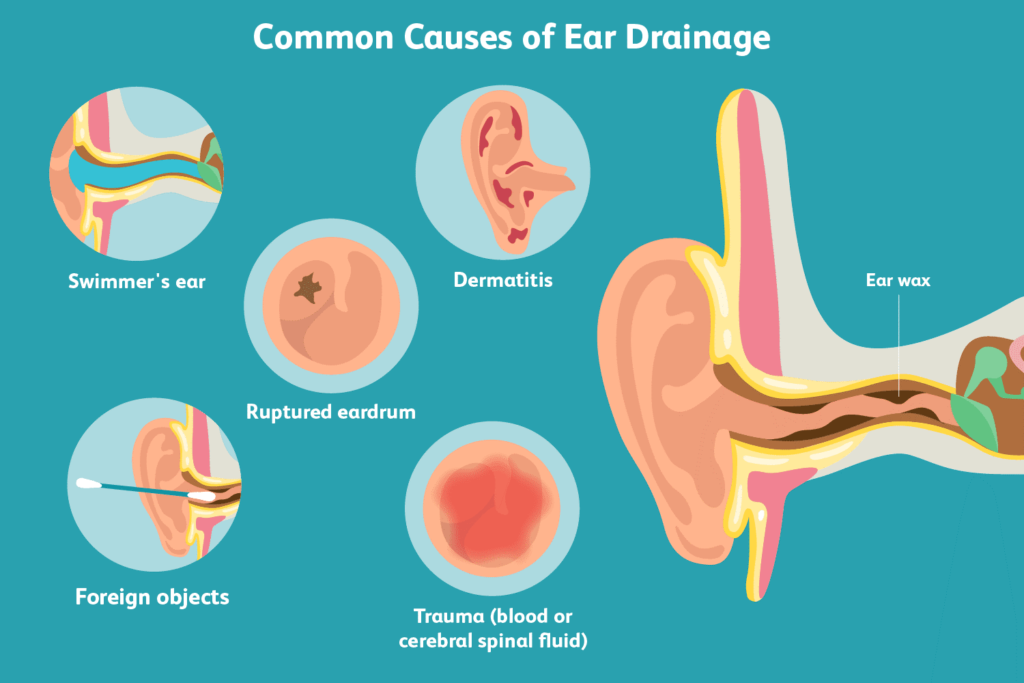 Anyone who has experienced drainage from their ear can tell you what an unpleasant experience it is. It can cause stains on your pillow or the collar of your shirt. It can be associated with hearing loss. It may even come with ear pain. It often leaves the sufferer wondering: what is leaking from my ear?
Anyone who has experienced drainage from their ear can tell you what an unpleasant experience it is. It can cause stains on your pillow or the collar of your shirt. It can be associated with hearing loss. It may even come with ear pain. It often leaves the sufferer wondering: what is leaking from my ear?
Otorrhea, the medical term for ear drainage, comes in many different forms. It may be clear, yellow, white, or bloody. It may be odorless or have a foul odor. It can be thin and watery or thick like mucous.
It has as many different causes as its different characteristics. If you are a swimmer, the frequent exposure to water can lead to chronic moisture retention. The skin of the ear canal becomes infected and as the skin weeps, otorrhea develops. Trauma to the skin by aggressive ear cleaning can result in a similar infection of the ear canal. If you have diabetes and ear drainage a more serious infection can quickly develop.
If you have a history of chronic ear infections, perforation of the ear drum allows for drainage of pus from the middle ear (space behind the ear drum). Chronic ear infections can also cause a skin cyst to develop in the middle ear (cholesteatoma). Recurring episodes of foul smelling otorrhea that improve temporarily with antibiotics only to come back suggests cholesteatoma. Blood from the ear may also be seen in this condition.
Rarely, clear fluid leaking from the ear is brain and spinal fluid (CSF). A history of ear surgery increases the concern for clear fluid being serious. CSF leaking from the ear indicates a hernia between the brain and ear (encephalocele). Untreated CSF leak can cause chronic headaches. Repair is needed to stop the leakage and remove the possibility of brain infection (meningitis).
 Have you ever heard a sound that no one else hears? You are not alone. There are many sounds that can be heard in the ears or head. Some are benign. Others may be need to be evaluated. All can be concerning if you have never experienced a sound no one else hears.
Have you ever heard a sound that no one else hears? You are not alone. There are many sounds that can be heard in the ears or head. Some are benign. Others may be need to be evaluated. All can be concerning if you have never experienced a sound no one else hears.
One category of sounds in the ear is tinnitus. Tinnitus is very common. It affects almost one in five people. It becomes more prevalent the older you are. It is associated with both hearing loss and acoustic trauma. It may sound like buzzing, humming, whistling, birds, insects, etc. Although it is often perceived in the ear, current science suggests it is generated in the central nervous system.
In healthy ears, hearing cells within the inner are connected to nerves that transmit sound from the ear to the brain. Although hearing cells are destroyed with hearing loss, the nerves deeper in the brain are not always lost. These nerves no longer receive stimulation, and begin to create signals on their own. Because these signals are not generated from the outside world, we perceive sound that no one else does.
Tinnitus, therefore, is a sign that hearing loss has occurred. It often occurs after a loud concert, sports event, or work experience. Tinnitus that occurs in only one ear or occurs with episodes of dizziness is more concerning than tinnitus that occurs in both ears over many years.
Some tinnitus sounds like whooshing and occurs with your heart beat. This is called pulsatile tinnitus. Normally our ear is protected from hearing internal blood flow. Medical conditions may decrease the shielding of our ear from internal sounds. Hearing your pulse only on your pillow, however, is not abnormal.
Wax or fluid in the ear may increase the resonance of blood flow making it audible. Weight loss may leave the Eustachian tube stuck open causing audible breathing sounds and heart sounds. Hernia of the brain into the ear also causes awareness of one’s heartbeat.
Other conditions increase the blood flow above normal levels. Head trauma may result in aneurysm or fistula of blood vessels near the ear. Vascular tumors may increase blood flow around the ear. Anemia and dehydration increase the force of the heartbeat resulting in pulsatile tinnitus. Some medications may increase brain pressure and cause pulsatile tinnitus.
A rare cause of thumping sound in the ear is muscle twitching. Muscles attached to the hearing bones or the Eustachian tube will make a thump when they contract. Just like a muscle twitch can occur in the eye lid, a muscle twitch of these muscles can occur and will cause a rapid thumping sound.
Crackling or popping is normal to occur with chewing, swallowing, or yawning. Excessive crackling or popping may be due to a Eustachian tube that is stuck closed.
Noisy ears associated with hearing loss or dizziness should be evaluated. Pulsations that are persistent should also be evaluated.
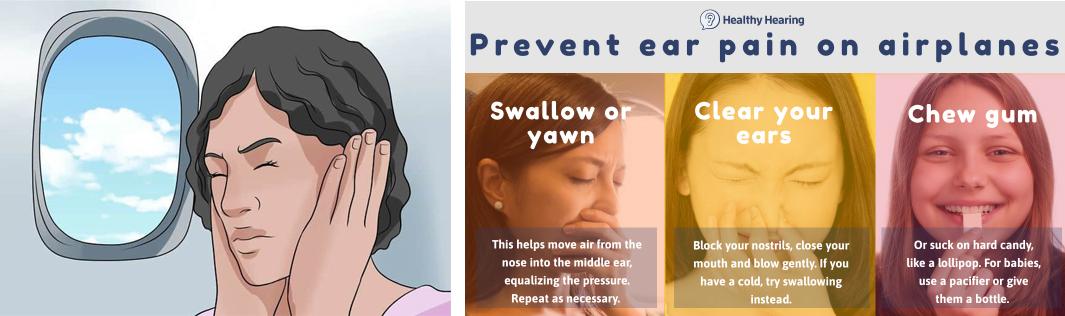
Flying can be difficult for your ears. Problems that arise during or after flying are helped by understanding them. There are some easy tips that can prevent them all together.
Most problems are related to the Eustachian tube. It is a paired structure (one for each ear) that connects the middle ear (behind the eardrum) to the nasopharynx (a recess behind your nasal cavity at the top of your throat). The Eustachian tube acts as a valve to regulate pressure in the middle ear. The valve is opened by moving particular muscles in the head and neck. Swallowing, chewing, and yawning activate these muscles.
If the Eustachian tube stays closed during a major change in ambient pressure, trauma occurs in the middle ear. Major changes in pressure occur during ascent and descent during flight. Symptoms include ear pain/pressure, hearing loss, tinnitus, and dizziness.
Vestibular problems also occur during flying due to turbulence. There are limited visual cues in the cabin of a commercial jet. This can be disorienting. Coupled with significant forces exerted on the vestibular system during turbulence may cause motion sickness in sensitive individuals. These same individuals will often suffer from sea sickness and car sickness as well. The stimulation can leave the vestibular system sensitive even after the flight, resulting in the illusion that one is still on the plane.
Eustachian tube problems can be prevented by following these guidelines, especially during descent.
- Make sure you are awake. This keeps you aware of any changes in pressure.
- Chew gum. This makes sure you are chewing and swallowing.
- If you still feel discomfort, pinch your nose and blow against your closed nostrils gently. You will feel your ears equalize. This will be accompanied by an increased awareness of ambient sound.
If these measures do not work, you may need to see your doctor about a nasal decongestant or even placement of a ventilation tube in your eardrum.
