Nose
Rhinitis - What it is?
Rhinitis is a condition where the mucous membrane in the nasal cavity is inflamed.
Surgical
Symptoms of rhinitis include:
- Sneezing
- Nasal obstruction
- Sensation of a stuffy nose
- Runny nose
It is a common condition that may be caused by an infection, an allergic response or even overuse of certain medications.
Infective rhinitis is usually caused by viruses and results in the common cold.
Rhinitis – Treatments
Infections usually resolve on their own over a few days. Medical treatment is usually targeted at symptom relief. Antihistamines or nasal decongestants may be prescribed to alleviate symptoms of the disease.
Nasal decongestants like oxymetazolin, work by constricting the blood vessels in the mucosal lining. It is important to note that prolonged use of such decongestants may result in rebound symptoms (return of symptoms being treated which is now more severe than before) and worsening of the nasal obstruction. This is a condition known as rhinitis medicamentosa.

Overview
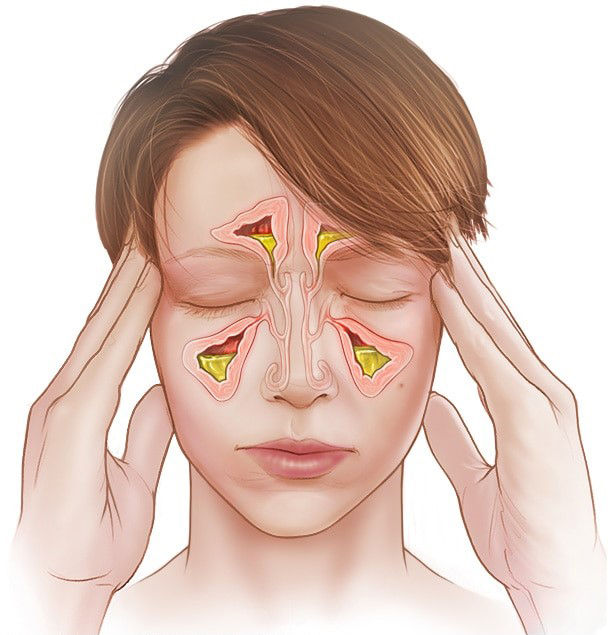
Acute sinusitis causes the spaces inside your nose (sinuses) to become inflamed and swollen. This interferes with drainage and causes mucus to build up.
With acute sinusitis, it might be difficult to breathe through your nose. The area around your eyes and face might feel swollen, and you might have throbbing facial pain or a headache.
Acute sinusitis is mostly caused by the common cold. Unless a bacterial infection develops, most cases resolve within a week to 10 days and home remedies may be all that’s needed to treat acute sinusitis. Sinusitis that lasts more than 12 weeks despite medical treatment is called chronic sinusitis.
Symptoms
Acute sinusitis symptoms often include:
- Thick, yellow or greenish discharge from the nose or down the back of the throat (postnasal drainage)
- Nasal blockage or congestion, causing difficulty breathing through your nose
- Pain, tenderness, swelling and pressure around your eyes, cheeks, nose or forehead that worsens when bending over
Other signs and symptoms include:
- Ear pressure
- Headache
- Aching in your teeth
- Altered sense of smell
- Cough
- Bad breath
- Fatigue
- Fever
When to see a doctor
Most people with acute sinusitis don’t need to see a doctor.
Contact your doctor if you have any of the following:
- Symptoms that last more than a week or so
- Symptoms that worsen after seeming to improve
- A persistent fever
- A history of recurrent or chronic sinusitis
See a doctor immediately if you have signs or symptoms that may indicate a serious infection:
- Pain, swelling or redness around your eyes
- High fever
- Confusion
- Double vision or other vision changes
- Stiff neck
Sinusitis
Causes
Acute sinusitis is most often caused by the common cold, which is a viral infection. In some cases, a bacterial infection develops.
Risk factors
You may be at increased risk of getting sinusitis if you have:
- Hay fever or another allergic condition that affects your sinuses
- A nasal passage abnormality, such as a deviated nasal septum, nasal polyps or tumors
- A medical condition such as cystic fibrosis or an immune system disorder such as HIV/AIDS
- Exposure to smoke, either from smoking or through secondhand smoke exposure
Complications
Acute sinusitis complications are uncommon, and serious complications are rare. If they occur, complications might include:
- Chronic sinusitis. Acute sinusitis may be a flare-up of a long-term problem known as chronic sinusitis. Chronic sinusitis lasts longer than 12 weeks.
- Meningitis. This infection causes inflammation of the membranes and fluid surrounding your brain and spinal cord.
- Other infections. Uncommonly, an infection can spread to the bones (osteomyelitis) or skin (cellulitis).
- Vision problems. If the infection spreads to your eye socket, it can cause reduced vision or even blindness that can be permanent.
Prevention
Take these steps to help reduce your risk of getting acute sinusitis:
- Avoid upper respiratory infections. Try to stay away from people who have colds. Wash your hands frequently with soap and water, especially before your meals.
- Manage your allergies. Work with your doctor to keep symptoms under control.
- Avoid cigarette smoke and polluted air. Tobacco smoke and other pollutants can irritate and inflame your lungs and nasal passages.
- Use a humidifier. If the air in your home is dry, such as it is if you have forced-air heat, adding moisture to the air may help prevent sinusitis. Be sure the humidifier stays clean and free of mold with regular, thorough cleaning.
Diagnosis
Your doctor will feel for tenderness in your nose and face and look inside your nose, and can usually make the diagnosis based on the physical exam.
Other methods that might be used to diagnose acute sinusitis and rule out other conditions include:
- Nasal endoscopy. A thin, flexible tube (endoscope) with a fiber-optic light inserted through your nose allows your doctor to visually inspect the inside of your sinuses.
- Imaging studies. A CT scan shows details of your sinuses and nasal area. It’s not usually recommended for uncomplicated acute sinusitis, but imaging studies might help find abnormalities or suspected complications.
- Nasal and sinus samples. Laboratory tests aren’t generally necessary for diagnosing acute sinusitis. However, when the condition fails to respond to treatment or is worsening, tissue samples (cultures) from your nose or sinuses might help find the cause, such as a bacterial infection.
- Allergy testing. If your doctor suspects that allergies have triggered your acute sinusitis, he or she will recommend an allergy skin test. A skin test is safe and quick, and can help pinpoint the allergen that’s causing your nasal flare-ups.
Treatment
Most cases of acute sinusitis get better on their own. Self-care techniques are usually all you need to ease symptoms.
Treatments to relieve symptoms
Your doctor may recommend treatments to help relieve sinusitis symptoms, including:
- Saline nasal spray, which you spray into your nose several times a day to rinse your nasal passages.
- Nasal corticosteroids. These nasal sprays help prevent and treat inflammation. Examples include fluticasone (Flonase Allergy Relief, Flonase Sensimist Allergy Relief, others), budesonide (Rhinocort Allergy), mometasone (Nasonex) and beclomethasone (Beconase AQ, Qnasl, others).
- Decongestants. These medications are available in over-the-counter (OTC) and prescription liquids, tablets and nasal sprays. Use nasal decongestants for only a few days. Otherwise they may cause the return of more-severe congestion (rebound congestion).
- OTC pain relievers, such as acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) or aspirin.Use caution when giving aspirin to children or teenagers. Children and teenagers recovering from chickenpox or flu-like symptoms should never take aspirin. This is because aspirin has been linked to Reye’s syndrome, a rare but potentially life-threatening condition, in such children.
Antibiotics
Antibiotics usually aren’t needed to treat acute sinusitis. Even if your acute sinusitis is bacterial, it may clear up without treatment. Your doctor might wait and watch to see if your acute sinusitis worsens before prescribing antibiotics.
However, severe, progressive or persistent symptoms might require antibiotics. If your doctor prescribes an antibiotic, be sure to take the whole course, even after your symptoms get better. If you stop taking them early, your symptoms may recur.
